Bill Dixon, 80, lay on a bed between two white fabric dividers in the hallway of the emergency department at Scripps Memorial Hospital Encinitas Friday, one of 14 patients waiting for an emergency bed to open up.
He had been there for two hours, having come in from his Solana Beach home with chest pain and dizziness, comfortable with the attention he was getting from medical staff, but taken aback by his surroundings.
“This is really not acceptable from a patient perspective,” the Solana Beach resident said. “There’s really no privacy.”
On Friday, all 38 of the hospital’s emergency department rooms were full of patients, and 20 of them had already been admitted for overnight stays, but no beds were available in the main hospital, forcing them to hold up in emergency rooms.
It is a medical malaise the industry calls “boarding,” a phenomenon that local experts say could be exacerbated by a new state law that would broaden the set of circumstances when residents may be detained by law enforcement and brought to local emergency departments for evaluation. Because the new law expands the current definition of “gravely disabled” to include those “unable to provide for their personal safety or necessary medical care,” it is widely expected to most directly affect the unhoused.

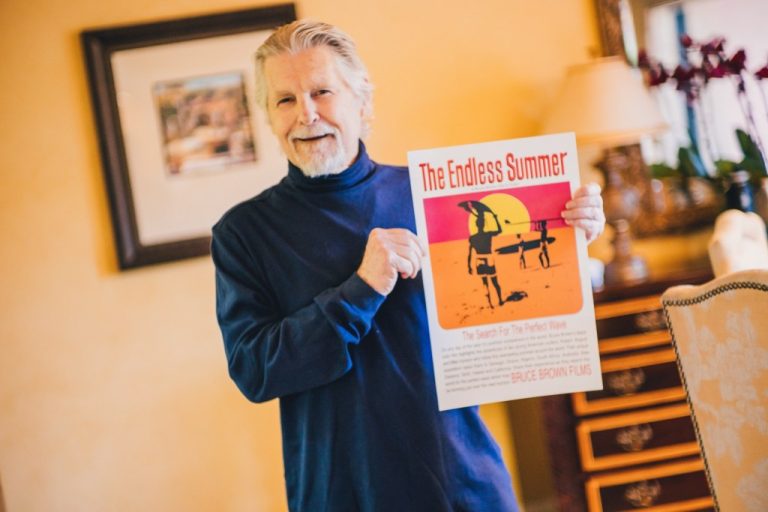
The emergency department hallways at Scripps Memorial Hospital held 14 patients Friday, Dec. 1, 2023, afternoon as the facility had 20 “boarding” patients who could not leave the ER because no beds were available in the main hospital.
(Alejandro Tamayo/The San Diego Union-Tribune)
Called Senate Bill 43, the new law, set to take effect Jan. 1, will be the subject of a county hearing Tuesday at which supervisors will debate delaying its implementation for one year. Some argue that taking more time would allow better planning to minimize impact on already crowded ERs while others, including the mayor of San Diego, argue that such a delay would be cruel to the thousands of people living on city streets who need help now.
Hospitals are stepping into the debate in a more vocal way than they usually do, warning that they simply do not have any extra capacity, especially during the busy winter months, which typically bring many additional patients sick with respiratory illnesses into their waiting rooms.
While local data on the overall prevalence of boarding, and its crowding effects on emergency room hallways, was not immediately available, this is a nationally recognized phenomenon.
The American College of Emergency Physicians recently called boarding in emergency departments a “national public health crisis,” releasing poll results that indicate “almost half of adults (43 percent) would delay or avoid going to the emergency department if they knew that they, or a loved one with a severe illness or injury, could face extreme delays associated with boarding.”
It is clear that not every hospital in San Diego is experiencing severe patient backups to the same extent that Scripps Encinitas has been. Larger Scripps facilities in Hillcrest and La Jolla were doing better with the issue last week. But at the same time, the problem has recently been so intense in some locations that it has spurred action. UC San Diego Health, for example, recently announced it had purchased Alvarado Hospital in La Mesa out of concern that its emergency departments had become clogged with overflow patients lodging for far too long in emergency hallways, converted waiting areas and even a re-purposed conference room.
Sharp HealthCare, the region’s largest medical provider, said that its four hospitals in San Diego, Chula Vista, La Mesa and Coronado have, on average, 35 emergency patients waiting for placement per day, and handled nearly 2,500 involuntary holds over the past 12 months. At the same time, those facilities have seen the number of emergency visits they handle in a year increase by 27,000 since 2022.
Across San Diego County, ERs are regularly holding many patients who should have already been moved to inpatient units. The Hospital Association of San Diego and Imperial Counties said that on Wednesday, Nov. 29, there were 187 boarders reported in emergency departments across the region. A total of 127 beds across all local hospitals were waiting to be discharged to skilled nursing facilities and, on average, between 50 and 70 patients per day were waiting to be discharged from behavioral health beds to long-term accommodations at “step down” facilities after completing hospital treatment.
What’s causing this multi-level gridlock?
Dr. Scott Eisman, chief operating executive at Scripps Encinitas, said that no one has fully explained the phenomenon, though it is has worsened since the COVID-19 pandemic.
“What may have happened to some degree is people with chronic illness, elderly patients, just couldn’t get a lot of care in the pandemic, and I think you’re still seeing a lot of that effect, that’s my hypothesis,” Eisman said.
And, he added, ERs are just the collection point for an entire system thrown off its rhythm. Many patients, he noted, are ending up waiting in hallways when they can’t get timely appointments to see their primary care doctors.

Dr. Scott Eisman, chief physician executive at Scripps Memorial Hospital Encinitas, talks with boarded patient Aaron DeLaby on Friday.
(Alejandro Tamayo/The San Diego Union-Tribune)
That was the case Friday for Aaron DeLaby, 63, a design engineer from Carlsbad who came in with pneumonia that just was not getting better, leaving him short of breath.
“For many weeks I was getting progressively worse,” DeLaby said. “The antibiotics didn’t work, just didn’t do anything, so I made an appointment with a pulmonologist to find out what the next step was, but they couldn’t get me in until Dec. 28.
“I wasn’t sure about being able to wait that long, and they said to go to the emergency room, so I did.”
His case, Eisman said, is a good example of the breadth of the problem.
“You know, it’s difficult right now to see doctors anywhere, not just in hospitals,” he said. “We don’t want to let him go home, we don’t want his disease to get worse, so we just have to do everything we can where we can.”
For DeLaby, that meant hours on a bed in the hallway before a private emergency examination room opened up. He spent the night in that room, continuing to lodge there into Friday afternoon.
Doctors and other medical professionals who generally work on inpatient units came to him for specialty consults, blood work, medical imaging and other services.
At the end of the day, he said, he didn’t mind his time in the hallway or staying over in the ER instead of getting a spot in a quieter unit more specialized to serving longer-term patients. But, he added, many of those on either side of him in the hallway Thursday were suffering more severe medical problems. Many were elderly and forced to share their medical histories out in the open.
“I didn’t really care that much about being out in the hallway, but I felt like I was sort of intruding on my neighbors,” DeLaby said. “You know, intruding on their stuff.
“You can’t help hearing it even though you don’t intend to listen.”